As parents and caregivers, it may feel natural to feel proud when our teens take an interest in healthy eating and exercise, especially in the world of competitive sports. You may even be envious of their willpower, especially if you have struggled with your own relationship to food and body image. However, this pride can quickly turn to concern when the new “healthy” habits become extreme, and the thinking becomes obsessive. It may even take you a while to wrap your mind around these perplexing changes in your teen. You may even experience some confusion about whether this is part of normal adolescence… or it is not…
Adolescents, especially teen athletes in weight-related sports, are particularly susceptible to eating disorders. The stakes are high to get into college, academics are stressful, and social media is relentless and insidious. For teen athletes, The pressure to perform, combined with societal and social media unrealistic and Eurocentric ideals around body image, plus any genetic predispositions, can create a perfect storm for these serious conditions to develop.
Early Warning Signs to Watch Out For
Paying attention to the early warning signs of eating disorders can lead to earlier intervention and better outcomes. Here are some red flags to watch for in your child:
20 Early Warning Signs of Eating Disorders in Teens:
- Eating, once carefree, becomes overly cautious
- Skipping meals, especially lunch at school
- Thinness without vibrancy
- Overconcern about nutritional content of foods
- Cutting our food groups deemed not to be “healthy”
- Rejection of the foods of one’s cultural heritage
- New reluctance to eat with family, friends, and in public
- Increasing preoccupation around body image, thinness, and a flat tummy.
- Connecting self-worth to body shape/size; unable to see one’s own beauty.
- Constantly comparing, fears about being teased, distorted negative body image.
- Delayed puberty or regression in puberty, such as amenorrhea
- Rapid plunge or increase in weight, regardless of starting body size or BMI.
- Adult-like mindset to “dieting”, disconnected from the need for a child or teen to grow and mature.
- Obsessive ritualistic behaviors around food, sneaking food, micro biting, etc.
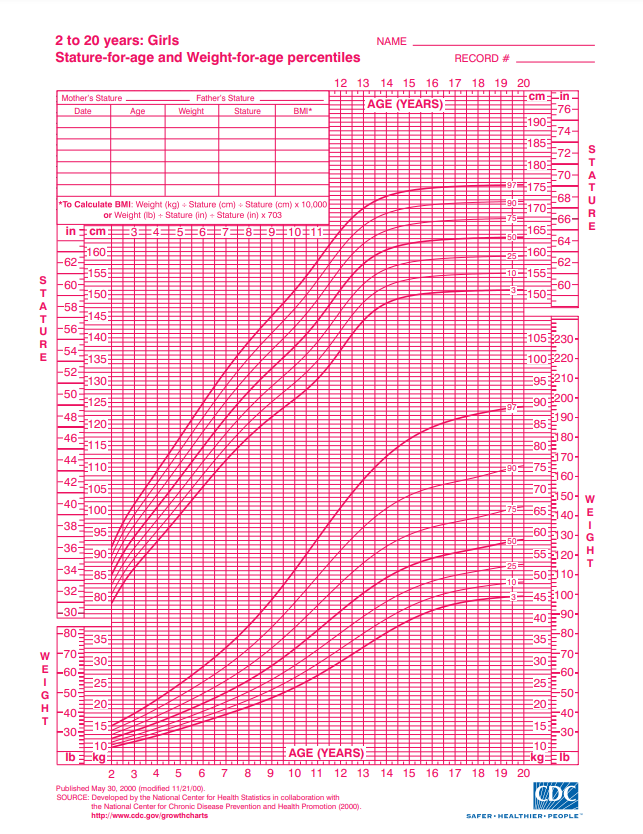
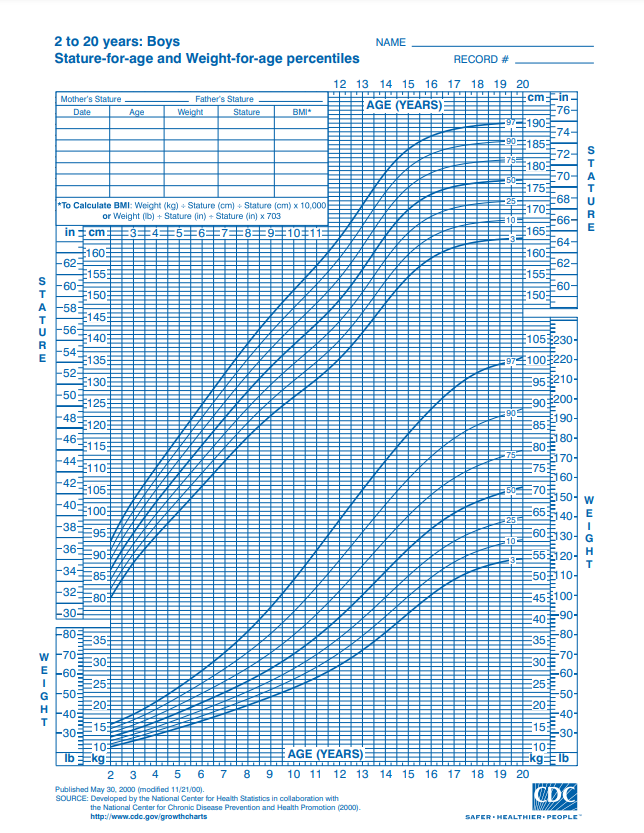
- Falling off one’s own growth curves; failure to reach Expected Weight/Height
- Excessive exercise with the intent to alter one’s natural body shape.
- “Picky”, selective eating that does not resolve.
- Bulimic symptoms – purging or using laxatives.
- Increase in anxiety, depression, even suicidal ideation
- Medical symptoms such as dizziness, fainting, low heart rate, low body temperature, weakness, gastric, and bowel discomforts
Eating Disorders remain one of the most lethal of the psychiatric illnesses. The medium onset of anorexia has dropped from 14 years of age to 12 years of age. Children as young as 6 years old are concerned about being “fat”. Boys and children from all ethnic/cultural backgrounds experience negative body image concerns. Bullying around body size and shape is now becoming the most common form of bullying in middle school.
Regardless of body size, Anorexia Nervosa and Bulimia Nervosa have serious medical and mental health consequences. Restrictive Eating Disorders will have medical complications that are the direct result of starvation and weight loss. Children and Adolescents who are diagnosed with Atypical Anorexia, are children who begin in larger bodies or higher weight bodies. These children can suffer the same if not more, from a severe and rapid plunge with weight loss. The heart and all organs are compromised with starvation, regardless of body size. The brain is one of the primary organs impacted by starvation, which impacts mood, anxiety, and mental health in general.
What are the dangers of dieting and restricting of intake in children and teens.

10 Reasons why Children should not Diet... Ever!
- Children and Adolescents follow a predictable pattern of growth that determines the growth and health of all organs, brain matter, and their entire skeletal system.
- Dieting and weight loss in children can have potential irreversible impact on both physical and emotional growth
- 40-60-% of peak bone mass is accrued during adolescents
- Compromised Bone Health can lead to a lifetime of increased fracture risk.
- Starving is damaging to the heart and causes bradycardia.
- Brain is under development until age 25. Emotional maturity can be stunted, as can growth
- During Puberty, nutritional and hormonal factors play a major development in Bone Development
- The oestrogens, Estrogen and Testosterone, are thought to play a key role in increasing and maintaining bone mass in adolescent males and females
- Anorexia and Bulimia can come with an increased risk of suicidal ideation
- Without proper intervention, an acute eating disorder turns into a chronic eating disorder
An Eating Disorder in Teens is characterized by a lot of ‘excuses’. “I am not hungry”. “I already ate”. I “This is not healthy” “I need to take a shower right after dinner. “No one eats lunch! it is not cool!” And food groups begin to drop off their list of acceptable foods…
Early Intervention is the Key – If you see an eating disorder specialist, especially one trained in FBT, they will help you intervene early in this process. The goal is to prevent acute symptoms from becoming chronic.
Around the Globe, Family Based Treatment is considered First-Line-of-Treatment
Family-Based Treatment (FBT)
Family-Based Treatment (FBT) has emerged, internationally, as one of the most effective methods for treating eating disorders in young people. This approach involves the family directly in the recovery process, empowering parents to guide their child back to health. Turning the ship around, back in the direction it came from, when eating was more carefree.
FBT is a protocol in 3 phases:
Phase 1 – Weight Restoration: The family takes control of the teen’s restrictive eating habits, by supervising and supporting fuller nutrition and intake to stop the downward weight loss spiral and begin to “weight restore”. Parents temporarily stop calorie –burning exercise and intervene with eating disorder symptoms, such as throwing food away, pushing food around the plate, or purging.
Parents lend their child their “Wise Mind” when their child’s thinking is so impaired and irrational.
Phase 2 – Begin to return control and choices to the adolescent:
After a teen has made a lot of progress returning to their own growth curve and is eating well, the control of their eating is gradually returned back to the teen ,with ongoing family support. Flexibility and exposure work is encouraged here. Reintroducing foods and eating in new places is encouraged. Full nutrition with all food groups represented here, is key .
Phase 3 – Establishing Healthy Independence: In phase 3, the focus shifts to establishing normal adolescent development and healthy, independent eating habits. Full mental and physical weight restoration occurs here. For a child or a teen, these numbers are a moving target. We are looking here for “State not Weight”, meaning full mental health recovery may need more than the minimum acceptable medical weight.
Families don’t cause eating disorders, they are the best allies of recovery
FBT, around the globe, is considered the Gold Standard for pediatric and adolescent eating disorders. A good eating disorder specialist will help you decide whether outpatient care is best for your child right now, or if you need a higher level of care, if this is assessed to be the best step for your child now. Either way, Eating Disorder Treatment, when done right, and done early, can lead to lasting and positive outcomes for your child.
Families don’t cause eating disorders, they are the best source of support. Don’t let an early acute course of an eating disorder become a chronic course. Your involvement can change this course.
Resilience Golden Rule for Early Intervention: Intervene!
For every pound your child loses, they move toward medical danger. For every pound your child's weight restores, they move away from medical danger.
Eating Disorders progress fast. Early Detection and Early Intervention is key. Do not delay – Seek Professional Evaluation today
Seeking Professional Evaluation:
If you suspect your child might be struggling with an eating disorder, it’s crucial to seek professional help immediately. Early intervention can make a significant difference in recovery and ensure a positive prognosis.
For more information or support, contact us at Resilience DBT & Eating Recovery (973) 783-2292 and visit our website at www.ResilienceTherapy.com. Our offices are at 33 Plymouth Street, Suite 105, Montclair, NJ 07042, Tel: (973) 783-2292. We offer telehealth treatment in states listed on our website. We offer resources, support, and guidance for families seeking intervention and support around their teens relationship to food and body image
Having an Eating Disorder is not a Choice…. But Recovery is!
Eating Disorder Awareness Week, 2024 Information is in Partnership with 2024 National Eating Disorders Awareness Week .This post is part of our commitment to raising awareness about eating disorders and urge early diagnosis and intervention, share this message, and let’s work together to keep our children safe and healthy.
Copyright © Resilience DBT & Eating Recovery, 2024
How do I begin?
Our team is dually and expertly trained in the Treatment of Eating Disorders and DBT for Mental Health. Our Evidenced-Based approaches include FBT, CBT-E, DBT-ED, and Comprehensive DBT for co-occurring mental health conditions. Our outpatient practice has helped Children, Teens and Adults achieve full Eating Disorder Recovery and Mental Health Stability for over 25 years.
1
Schedule your 15 minute free phone consultation
This phone screening is highly confidential to help determine if coming to the Resilience practice is the best course for you or your loved one.
2
Complete an Expert and Comprehensive Intake
During your intake appointment we will gather more information to identify your stressors and needs. And work with you to develop your resilience treatment plan.
3
Get connected with Your Personalized Care Team
Meet with a practitioner to get started on your journey of healing and wellness you know you deserve.